A 35-year-old man presented to the emergency department with altered mental status and bilateral tonic-clonic seizures. Due to a progressive decrease in consciousness, he was intubated for airway protection. The patient's relatives reported that he had used cocaine, leading to an initial suspicion of acute cocaine intoxication. However, a head CT scan without contrast revealed a hyperdense basilar artery sign without other signs of infarction (Figure 1). Furthermore, DWI-MR imaging revealed multiple areas of infarction within the vertebrobasilar arterial circulation (Figure 2). Despite not showing occlusion of vertebral or basilar arteries, cerebral angiographic imaging was performed. Unfortunately, the patient was not diagnosed with acute stroke timely and therefore did not receive appropriate treatment. Eventually, after a few months, he was diagnosed with brain death in the intensive care unit.
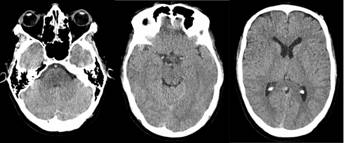
Figure 1 Head CT without contrast at admission. Head computerized tomography showing hyperdense basilar artery. However, there is no infarction, hemorrhage, or hydrocephalus. No intra-axial or extra-axial collection is present. Basal ganglia and posterior fossa structures are normal.

Figure 2 Brain MRI without contrast on day one of hospitalization. Brain MRI showing restricted diffusion on diffusion-weighted imaging in the right cerebellar lobule (Panel A), bilateral mesencephalon and left posterior cerebral lobe (Panel B), and left thalamus (Panel C) demonstrating multi-territorial infarcts in the posterior circulation.
Stroke misdiagnosis is common in young patients without vascular risk factors.(1) Moreover, cocaine use should not be considered a seizure risk factor, warranting further diagnostic studies.(2) Lastly, some patients with cocaine-induced stroke may have routine cerebral angiography due to the vasoconstriction-induced infarction mechanism.(3) In this patient, premature closure bias based on clinical and radiological features of cocaine-induced stroke resulted in delayed diagnosis.














