INTRODUCTION
According to the World Health Organization, accidental falls are a leading cause of non-fatal and fatal injuries in older adults, accounting for more than 37 million cases severe enough to require medical attention, and almost 700,000 case-fatalities annually.(1) The vast majority of these cases occur in Low- and Middle-Income Countries (LMIC), where the risk factors for falls differ from those observed in High Income Countries (HIC). This is particularly evident in rural settings where working conditions with poor safety standards and inadequate housing contribute to an increased risk of falls.(2) A recent cross-sectional study conducted among community-dwelling older adults living in Atahualpa, a rural Ecuadorian village,(3) demonstrated a high frequency of falls in the year prior to the study (53%) despite a disproportionately theoretically low risk of future falls (27%) according to the Downton Fall Risk Index (DFRI). The DFRI is a field instrument constructed to predict the risk of future falls according to history of falls and clinical characteristics of individuals at baseline.(4)
In view of the scarcity of healthcare resources in remote rural communities of LMIC, an accurate estimate of the actual risk of future falls is important for planning cost-effective strategies aimed at reducing the risk of falls as well as addressing their consequent morbidities in these vulnerable populations. The DFRI has mostly been used in HIC and fails to adequately consider the impact of environmental factors that contribute to the actual risk of future falls among people living in rural villages of LMIC.(4)(5)(6)(7) For this reason, the predictive value of the DFRI may not be reliable in these settings. Even in HIC, some studies have failed to corroborate the validity of this field instrument, and a recent meta-analysis found a relatively low reliability of the DFRI for predicting the risk of future falls.(8)(9)
There is no longitudinal data on the accuracy of the DFRI in predicting falls among community-dwelling older adults living in rural settings. Utilizing baseline data from the previously mentioned cross-sectional study conducted in Atahualpa,(3) we examined the reliability of the DFRI as a predictor of incident falls during three years of prospective follow-up.
METHODS
Study population: The study was conducted in community-dwellers aged ≥60 years living in Atahualpa, a rural village located in coastal Ecuador. Inhabitants are homogeneous regarding ethnicity (Amerindian ancestry), low levels of education, poor socio-economic status, and dietary habits, as detailed elsewhere.(10) The diet is rich in oily fish, fruits and carbohydrates, but restricted in other types of meat, dairy products, and highly processed foods. Physical activity is satisfactory, since most residents mobilize within the village by walking or bicycle riding, as very few own a motor vehicle. Figure 1 shows characteristics of the village. Most streets are non-paved and became muddy during the rainy season. In addition, many houses have architectural barriers such as unsafe steps, narrow doors and small bathrooms. About 20% of houses have open latrines with humid and uneven floor surfaces. The village has only one public health center staffed by general physicians, nurses, odontologists, and obstetricians. (Figure 1)

Figure 1 Characteristics of Atahualpa, depicting non-paved streets, houses with architectural barriers and open latrines, all providing scenarios that favor the occurrence of accidental falls.
Study design: Atahualpa residents aged ≥60 years identified by means of annual door-to-door surveys and enrolled in the Atahualpa Project from June 2012 to May 2018 were invited to participate, and those who remained actively enrolled in the cohort as of January 2019 and signed a comprehensive informed consent were considered eligible for follow-up. Interviews and procedures at enrolment aimed to assess demographics, alcohol intake, cardiovascular risk factors, and history of an overt stroke. During the first two months of 2019 a structured questionnaire was applied to evaluate history, severity, and circumstances surrounding accidental falls. In addition, the risk of future falls was assessed by means of the DFRI.(3) Individuals participating in the baseline study were followed for three years in order to assess the reliability of the baseline DFRI for predicting the actual risk of incident falls.
During the course of the study, Atahualpa residents were periodically visited at their homes to update information about their continued residence in the village and the occurrence of any incident strokes. At the end of the follow-up period (March 2022), a falls assessment questionnaire was again administered to those individuals remaining in the active cohort. Research staff who carried out the follow-up questionnaire were blind to the results of baseline assessments. Individuals who emigrated, declined consent, died during the study years or who suffered an incident stroke were excluded from the final analysis. The study followed the recommendations of the standards for reporting of observational longitudinal studies in epidemiology (STROBE) guidelines.(11) The study protocol and informed consent forms were approved by the I.R.B. of our Institution.
Falls assessment: A structured questionnaire was used for baseline falls assessment. As detailed elsewhere,(3) this questionnaire consists of four questions: 1) Have you experienced an unintentional fall in the year before this test (if positive, how many falls can you recall); 2) What was (were) the most likely cause(s) of the fall(s)?; 3) Did a fall resulted in hospitalization?; and 4) Were there any bone fracture(s) due to a fall? (specify which bones). At follow-up, a similar questionnaire was given to all participants, the only difference being that the follow-up exam inquired about falls during the previous three years. The risk of future falls was estimated - at baseline - by the DFRI, a five-question instrument that ascertains the history of previous falls, the use of specific medications (tranquilizers/sedatives, diuretics, non-diuretic anti-hypertensives, anti-parkinsonians, and antidepressants), any sensory or motor deficits (visual impairment, hearing impairment, paresis), gait abnormalities (with or without aid or impossible), and the presence of confusion.(4)(6) A score ≥3 points in the DFRI indicates an elevated risk for future falls. The analysis also takes into account the continuous DFRI score.
Covariates investigated: Age, sex, level of education, severity of alcohol intake, cardiovascular risk factors, and prevalent overt strokes were selected as covariates of interest, and were assessed by means of interviews and procedures previously described in the Atahualpa Project.(10) These covariates were identified as they have been shown to modify fall risk in similar studies conducted in other regions.(12) In order to assess traditional cardiovascular risk factors, the American Heart Association criteria were used to define poor physical activity, body mass index, and blood pressure levels.(13) Alcohol intake was classified as severe if >50g per day. To identify prevalent overt stroke cases (at baseline), all participants were screened by rural doctors with the use of a validated field questionnaire, and then, certified neurologists confirmed the diagnosis with the aid of a brain MRI.
Statistical Analyses: Descriptive statistics are presented as means with standard deviations for continuous variables and as percentages with 95% confidence intervals (C.I.) for categorical variables. Logistic regression models were fitted to assess the relationship between the DFRI (dichotomized and continuous) and incident falls, after adjusting for the aforementioned covariates. Reliability of a positive DFRI to predict incident falls was assessed by calculating its sensitivity and specificity, as well as its positive and negative predictive values. Using receiver operator characteristics (ROC) curve analysis, we calculated the area under the curve (AUC) for the trustworthiness of a positive DFRI to predict incident falls. In addition, reliability of history of falls (as a single exposure variable instead of a positive DFRI) to predict incident falls was calculated by means of a different ROC curve analysis and AUC calculation. All analyses were carried out by using STATA version 17 (College Station, TX, USA).
RESULTS
A total of 327 (71%) out of 463 individuals aged ≥60 years enrolled in the Atahualpa Project cohort from 2012 to 2018 had baseline interviews to document previous accidental falls and to estimate the risk of future falls. Among the 136 excluded individuals, 68 died, 15 emigrated between enrollment and the invitation for these interviews, and the remaining 53 declined consent. At baseline, three additional subjects were not ambulatory and therefore excluded from the cohort. Excluded individuals were older and had worse physical activity than those eligible for follow-up. Otherwise, there were no differences across groups (Table 1).
Table 1 Characteristics of Atahualpa residents aged ≥60 years identified by means of door-to-door surveys according to whether they were excluded or considered eligible candidates for the follow-up.
| Excluded individuals (n=139) | Eligible for follow-up (n=324) | p value | |
|---|---|---|---|
| Age, years, mean±SD | 74.4±10.4 | 70.3±8 | <0.001* |
| Women, n (%) | 73 (53) | 183 (56) | 0.432 |
| Primary school education, n (%) | 111 (80) | 250 (77) | 0.521 |
| Body mass index ≥30 kg/m2, n (%) | 31 (22) | 77 (24) | 0.733 |
| Poor physical activity, n (%) | 28 (20) | 27 (8) | <0.001* |
| Hypertension, n (%) | 71 (51) | 139 (43) | 0.105 |
| Severe alcohol intake, n (%) | 14 (10) | 52 (16) | 0.092 |
| Stroke at baseline, n (%) | 11 (8) | 22 (7) | 0.667 |
*Statistically significant result
Follow-up assessments were possible in 270 (83%) of 324 individuals eligible at baseline. The others died (n=51), emigrated or declined consent (n=3) during the follow-up. In addition, 16 individuals developed an incident stroke and were not included in analysis due to a potential increased risk of falls that could have not been predicted by the baseline DFRI. Figure 2 shows the reasons for exclusion of participants at each stage of the enrollment process. Follow-up time between baseline and follow-up assessments was 803 person-years (95% C.I.: 802 - 804 years) in the 254 individuals who completed the study. The mean person-years of follow up was 3.2 years with a standard deviation of ±0.04. (Figure 2)

Figure 2 Flow chart showing enrollment and the reasons for excluding participants at each stage of this process.
At baseline, the mean age of 254 participants was 68.9±6.9 years, 146 (57%) were women, and 192 (76%) had primary school education only. Sixty-three (25%) subjects had a body mass index ≥30 kg/m2, 15 (6%) had no vigorous or moderate physical activity, 101 (40%) had blood pressure levels ≥140/≥90 mmHg, 44 (17%) had severe alcohol intake, and 15 (6%) had an overt stroke (confirmed by MRI). Also at baseline, a history of falls in the year prior was recalled by 135 (53%) individuals. Of these, 107 (79%) had only one or two fall episodes. Falls most often occurred outdoors and were almost always related to stumbling due to irregularity of the non-paved streets or bicycle falls. Indoors falls were often linked to bed or hammock falls. Less common causes for outdoors or indoors falls included alcohol intoxication, motor weakness and syncope. None of these individuals needed hospitalization after the fall and no individual had bone fractures as the result of the fall. The mean DFRI score in the entire population was 1.6±1.3 points (range: 0 to 6 points), with 54 (21%) individuals having an increased risk of future falls (DFRI score ≥3 points).
A total of 158 (62%) individuals experienced one or more falls during the follow-up (mean number of falls: 2.7±2.4; range: 1 to 18 falls). Sixteen individuals required hospitalization for falls, which were related to bone fractures in 50% of cases. Bone fractures involved the wrist/fingers in three cases, the shoulder girdle in two, the forearms in two, and the ankle in the remaining subject. There were no cases of skull bones or hip fractures nor fall-related deaths in our population. Comparison of clinical characteristics across individuals who had incident falls versus than those who did not, showed that previous strokes, history of falls, the baseline DFRI score and the number of individuals with a positive DFRI were significantly different across groups in unadjusted analyses (Table 2). A multivariate logistic regression model that used a positive DFRI as the exposure (independent variable) and incident falls as the outcome (dependent variable) showed that individuals with a positive DFRI have a fivefold increase in the rate of incident falls than those without history of falls (OR: 4.91; 95% C.I.: 1.94 - 12.4; p=0.001). None of the covariates used for adjustment remained independently significant in this model, but previous strokes attained a marginal significance (p=0.062) (Table 3). A separate multivariate logistic regression model that used the continuous DFRI score as the exposure and incident falls as the outcome also showed a significant association between the main investigated variables (OR: 1.56; 95% C.I.: 1.18 - 2.06; p=0.002), which was clearly evidenced as increased average proportions of incident falls among individuals with two or more points in the DFRI score (Figure 3).
Table 2 Factors influencing the occurrence of incident falls among 254 individuals included in this study (unadjusted analyses).
| No incident falls (n=96) | Incident falls (n=158) | p value | |
|---|---|---|---|
| Age, years, mean±SD | 68±6.4 | 69.4±7.2 | 0.119 |
| Women, n (%) | 50 (52) | 96 (61) | 0.175 |
| Primary school education, n (%) | 75 (78) | 117 (74) | 0.464 |
| Body mass index ≥30 kg/m2, n (%) | 25 (26) | 38 (24) | 0.722 |
| Poor physical activity, n (%) | 5 (5) | 10 (6) | 0.713 |
| Hypertension, n (%) | 33 (34) | 68 (43) | 0.171 |
| Severe alcohol intake, n (%) | 19 (20) | 25 (16) | 0.418 |
| Stroke at baseline, n (%) | 1 (1) | 14 (9) | 0.011* |
| History of falls, n (%) | 3 (3) | 134 (85) | <0.001* |
| DFRI§ score at baseline, mean±SD | 1.1±1 | 1.8±1.4 | <0.001* |
| DFRI positive‡ at baseline, n (%) | 7 (7) | 47 (30) | <0.001* |
*Statistically significant result. § DFRI: Downton Fall Risk Index. ‡ DFRI positive means a score of ≥3 points.
Table 3 Logistic regression model showing a significant association between a positive Downton Fall Risk Index (≥3 points) and incident falls (outcome) in the study population.
| Incident falls | Odds ratio | 95% C.I. | p value |
|---|---|---|---|
| Positive Downton Fall Risk Index | 4.91 | 1.94 - 12.4 | 0.001* |
| Age at baseline | 1.00 | 0.96 - 1.05 | 0.904 |
| Being women | 1.51 | 0.78 - 2.91 | 0.224 |
| Primary school education | 0.74 | 0.39 - 1.42 | 0.367 |
| Body mass index ≥30 kg/m2 | 0.82 | 0.42 - 1.61 | 0.571 |
| Poor physical activity | 0.69 | 0.19 - 2.46 | 0.568 |
| Arterial hypertension | 0.99 | 0.56 - 1.79 | 0.996 |
| Severe alcohol intake | 1.12 | 0.48 - 2.61 | 0.800 |
| Stroke at baseline | 7.56 | 0.91 - 63.04 | 0.062 |
*Statistically significant result
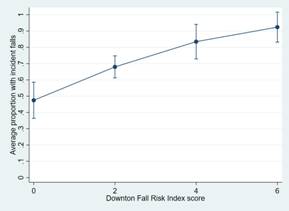
Figure 3 Graph plot showing average proportions of incident falls according to scores in the Downton Fall Risk Index at baseline.
ROC analysis revealed that a positive DFRI has a sensitivity of 29.7% (95% C.I.: 22.8% - 37.6%), a specificity of 92.7% (95% C.I.: 85.1% - 96.8%), a positive predictive value of 87% (95% C.I.: 74.5% - 94.2%), and a negative predictive value of 44.5% (95% C.I.: 37.5% - 51.7%) for the occurrence of incident falls. The AUC for the predictive value of incident falls given a positive DFRI was 0.612 (95% C.I.: 0.568 - 0.657). A separate ROC analysis using only history of falls at baseline as the exposure (and not the DFRI) showed a sensitivity of 84.8% (95% C.I.: 78% - 89.8%), a specificity of 96.9% (95% C.I.: 90.5% - 99.2%), a positive predictive value of 97.8% (95% C.I.: 93.2% - 99.4%), and a negative predictive value of 79.5% (95% C.I.: 70.8% - 86.2%) for the occurrence of incident falls. The AUC for the predictive value of incident falls given a history of previous falls was 0.908 (95% C.I.: 0.875 - 0.942).
DISCUSSION
This longitudinal prospective cohort, conducted in community-dwelling older adults living in a remote rural community, showed significant associations between a positive DFRI as well as the continuous DFRI score and the occurrence of incident falls. Despite these results, however, the DFRI has a poor sensitivity and a low negative predictive value to predict incident falls, a finding that was confirmed by ROC curve analysis (AUC: 0.612). When only a history of previous falls was used for analysis, the predictive value of this variable was much higher (AUC: 0.908) than the total DFRI. Given that previous falls are a core component of the DFRI, this factor is likely the most important variable that accounts for the aforementioned associations. The other components of this field instrument, namely, use of medications, sensory or motor deficits, gait abnormalities and confusion, do not appear to have a major role as predictors of future falls in the study population.
Despite differences in study populations, two Swedish studies conducted in subjects hospitalized in geriatric units demonstrated that history of falls was the most relevant risk factors accounting for falls after discharge, even more predictive than the DFRI.(6)(7) As previously mentioned, reliability of the DFRI for predicting the risk of future falls has been questioned in a recent systematic review.(9) In that review, the pooled sensitivity of the DFRI was adequate (84%) while the pooled specificity was low (26%). The present study shows the opposite result, a sensitivity of about 30% and a specificity of nearly 93%. Such differences point to lack of consistence (reliability) of the DFRI when used for predicting the risk of future falls. For example, Moreover, another study found that the DFRI was inversely associated with the risk of future falls (at least in women).(14) These inconsistencies could have been not only related to heterogeneity of study populations but probably due to inconsistencies within the structure of the DFRI. As previously noted, the DFRI does not take into account environmental factors, which most likely contribute to a sizable percentage of falls among older adults.
With regard to the characteristics and severity of falls, results of this prospective cohort align with those of the previous cross-sectional study conducted in the same population.(3) Most individuals had one or two incident falls and only 5% had bone fractures. None of these fractures involved the hip or skull bones and there were no falls-related casualties in the study population. Hospitalization after a fall was rare. These characteristics are substantially different than those reported in other studies carried out in HIC and in residents of long care facilities.(4)(5)(6)(15)(16)(17) Overuse of sedatives and certain analgesics undoubtedly predispose older adults admitted to long-care facilities to falls and lead to worse outcomes. In the event of a fall, alert individuals are more likely to stretch their arms in an attempt to reduce the impact from the fall, and this may account for the lower severity of falls in the study population compared to settings such as long care facilities. None of the investigated clinical characteristics of study participants were significantly associated with incident falls, supporting the notion that falls in rural settings are not related to intrinsic conditions but to environmental factors. These results differ from those of a systematic review of articles from developed countries, where long term exercise was associated with fewer and less severe falls.(18) Such differences can be explained by the fact that only 6% of the study population have poor physical activity and the sample may be insufficient to find significant differences in analysis.
Major strengths of the present study include the longitudinal prospective population-based design with unbiased enrollment of participants as well as the systematic assessment of individuals by means of the same field instrument at baseline and follow-up. Homogeneity of the study population is, at the same time, a strength and a limitation of the study. It is a strength because it provides, for the first time, information on incident falls in community-dwellers of Amerindian ancestry living in remote rural villages; these results are particularly relevant for the millions of Amerindians living in similar conditions. At the same time, it is a limitation because our results cannot be generalized to other races/ethnic groups or to individuals living in long care facilities. Another limitation is the recall bias, since individuals were asked to remember history of falls in the three years prior the study.
In conclusion, the results of this study suggest that the DFRI is significantly associated with incident falls, but its predictive value is less than that of history of falls taken as a single variable. This is accounted for the fact that individuals may have a positive DFRI due to medication use and confusion without necessarily having a history of falls. It is possible that other field instruments used to predict the risk of future falls may be more accurate than the DFRI in remote rural settings. Further studies are warranted to identify more reliable methods for ascertaining the risk of falls in older adults living in underserved communities.