INTRODUCTION
Arterial hypertension is a major public health problem affecting almost one billion people worldwide. One of the main effects of arterial hypertension on the nervous system is related to the development of microangiopathy with damage of small perforating arteries resulting in recurrent strokes and cognitive decline.(1) A reliable biomarker of such damage is the presence of diffuse subcortical damage, also referred as white matter hyperintensities (WMH) of presumed vascular origin. (2) The impact of arterial hypertension (and other cardiovascular risk factors) on WMH progression has been investigated in several clinical series and population-based studies, but results are inconclusive. (3)(4)(5)(6)(7) Heterogeneity in study designs probably accounted for such differences. Moreover, most studies have been conducted in urban centers of developed countries, where cardiovascular risk factors are different than those observed in remote rural settings. More information from people of different races/ethnic groups who live in underserved communities is warranted to establish the role of high BP on structural brain damage in these individuals. Taking the opportunity of the population-based Atahualpa Project Cohort, this longitudinal prospective study aimed to assess the impact of high BP on WMH progression in community-dwelling older adults of Amerindian ancestry living in rural Ecuador.
METHODS
Study population: Characteristics of Atahualpa’s residents have been described elsewhere. (8) The population is homogeneous regarding race/ethnicity (Amerindian ancestry), socio-economic status, lifestyles, and dietary habits. Also, migration is limited and compliance with the study is high, which makes the village an optimal setting for the conduction of longitudinal studies.
Study design: Following a longitudinal prospective design, individuals aged ≥60 years who had a brain MRI and evaluation of cardiovascular health (CVH) metrics between 2012 and 2019, and were actively participating in the Atahualpa Project Cohort as of May 2021, were invited to receive a follow-up brain MRI. Study participants had been identified by means of door-to-door surveys and had signed a comprehensive informed consent before enrollment. Individuals signed a new informed consent before the practice of follow-up MRIs. The study was approved by the Ethics Committee of Hospital-Clínica Kennedy, Guayaquil (FWA 00030727). WMH progression was evaluated according to BP levels and other CVH metrics in the poor range at baseline.
Study procedures: Both baseline and follow-up MRIs were performed with the same equipment (Philips Intera 1.5T; Philips Medical Systems, Eindhoven, the Netherlands) following a previously defined protocol. (9) Interest focused on the presence and severity of WMHs, which were defined as lesions appearing hyperintense on T2-weighted images that remained bright on FLAIR (without cavitation) and graded according to the modified Fazekas scale. This scale recognizes three degrees of WMH severity: mild, moderate, and severe, as detailed elsewhere. (10) Both baseline and follow-up MRIs were independently read by one neuroradiologist and one neurologist blinded to clinical information. Kappa coefficients for interrater agreement of WMH severity were higher than 0.90 (at baseline and follow-up), and discrepancies were resolved by consensus. WMH progression was defined as the increase in at least one grade of the Fazekas scale in the follow-up MRI (Figure 1).
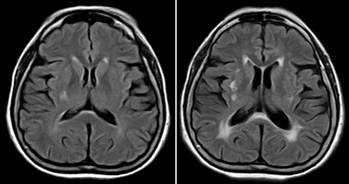
Figure 1 Fluid-attenuated inversion recovery MRI (TR 9000, TE 120, TI 2500) of a 62 year-old man showing progression of white matter hyperintensities from baseline MRI (left) performed in February 2014, to follow-up MRI (right) performed in May 2021.
Demographics and level of education were recorded at the time of baseline MRI. CVH metrics determination followed the recommendations and cutoffs proposed by the AHA. (11) The AHA stratify each of these CVH in the poor range according to well-defined cutoffs, including: 1) Poor smoking status if the subject is a current smoker or quit <1 year; 2) Poor body mass index if ≥30 kg/m2; 3) Poor physical activity if there is no moderate and vigorous activity; 4) Poor diet if there is none or only one of the following healthy dietary components: ≥4.5 cups fruits and vegetables/day, ≥two 3.5-oz servings fish/week, ≥three 1-oz equivalent servings fiber-rich whole grains/day, <1,500 mg sodium/day, and ≤450 kcal sugar-sweetened beverages/week; 5) Poor BP if ≥140/90 mmHg; 6) Poor fasting glucose if ≥126 mg/dL; and 7) Poor total cholesterol blood levels if ≥240mg/dL.
Interviews and procedures for CVH metrics determinations in the Atahualpa Project have been detailed elsewhere. (8) In particular, BP was measured by trained medical students with the use of a manual sphygmomanometer (Welch Allyn Tycos© 7670-01). Individuals were instructed to avoid food, coffee and cigarette smoking for at least one hour before BP determinations. With the person in the sitting position and after resting for 10 minutes, BP was measured in both arms and the mean value of three readings taken at intervals of two minutes (in the arm with the highest reading) was used for analysis.
Statistical analysis: Data analyses were carried out by using STATA version 17 (College Station, TX, USA). Multilevel ordinal logistic regression models were fitted to assess the risk of WMH progression in the follow-up (as the dependent variable) according to stratified levels of BP and other CVH metrics. In addition, separate multivariate logistic regression models were fitted to assess the impact of pulsatile and steady components of BP (as continuous values) and WMH progression at follow-up. These analyses took into account the longitudinal nature of the data and the fact that some patients already had WMH at baseline MRI.
RESULTS
A total of 403 (84%) out of 478 individuals aged ≥60 years enrolled in the Atahualpa Project cohort received a baseline MRI of the brain and clinical interviews. Among the 75 excluded individuals, 36 died or emigrated before the MRI, 19 declined consent, 17 were severely disabled or had contraindications for MRI, and three had missing clinical information. Of 403 eligible candidates, 263 (65%) had a follow-up MRI and were included in the study. Ninety of the 140 non-included participants died, and the remaining 50 either declined further consent, became disabled, or emigrated from the village between baseline and follow-up MRI. The total time of follow-up between baseline and follow-up MRIs was 1,711 person-years (95% C.I.: 1,665 - 1,757 years), and the median follow-up was 6.5 years (interquartile range: 2.3 - 7.8 years).
The mean (±SD) age of 263 study participants at the time of baseline MRI was 65.7±6.2 years (median age: 63.9 years), 149 (57%) were women, and 192 (73%) had primary school education only. High BP (≥140/90 mmHg) was recorded in 104 (40%) individuals (less than 30% of them were taking antihypertensive medications, often at suboptimal doses). Mean values of the different components of BP were: 138.9±23.7 for systolic pressure, 76.4±11 for diastolic pressure, and 63±20.2 for pulse pressure. Other individual CVH metrics in the poor range included: smoking status: 11 (4%); body mass index: 63 (24%); physical activity: 12 (5%); diet: 11 (4%); fasting glucose: 72 (27%); and total cholesterol blood levels: 41 (16%).
On baseline MRI, 90 (34%) participants did not have WMH, 131 (50%) had mild WMH, 33 (13%) had moderate WMH, and nine (3%) had severe WMH. At follow-up, 52 (20%) individuals did not have WMH, 112 (43%) had mild WMH, 67 (25%) had moderate WMH, and 32 (12%) had severe WMH. Overall, 103 (39%) individuals had MRI evidence of WMH progression. Progression from none-to-mild was noticed in 33 cases, from none-to-moderate in five, from mild-to-moderate in 42, from mild-to-severe in 10, and from moderate-to-severe in 13. In unadjusted analysis, people who had WMH progression were older (67.9±6 versus 64.3±5.8 years; p<0.001) and were less often obese (17% versus 29%; p=0.023) than those who did not have WMH progression; otherwise, there were no significant differences in clinical characteristics of study participants across groups.
By the use of a multilevel ordinal logistic regression model (using subjects with normal BP at baseline as the referent category), progression of WMH from baseline to follow-up increased 3.45 times (95% C.I.: 1.94 - 4.96) among non-hypertensive individuals and up to 6.15 times (95% C.I.: 3.18 - 9.12) among those with arterial hypertension. However, this difference was not significant due to overlapping of 95% confidence intervals (Table 1). Likewise, separate logistic regression models using individual components of BP as independent variables did not show any effect of these components on WMH progression at follow-up.
Table 1 Multilevel ordinal logistic regression model showing a non-significant progression of white matter hyperintensities (WMH) from baseline to follow-up visits according to levels of blood pressure.
| WMH progression | β coefficient | 95% C.I. | p value |
|---|---|---|---|
| Baseline visit # normal blood pressure | Referent category | ||
| Baseline visit # high blood pressure | 1.39 | -0.38 - 3.16 | 0.124 |
| Follow-up visit # normal blood pressure | 3.45 | 1.94 - 4.96 | <0.001* |
| Follow-up visit # high blood pressure | 6.15 | 3.18 - 9.12 | <0.001* |
| Age at baseline | -0.05 | -0.13 - 0.03 | 0.193 |
| Being female | 0.56 | -1.14 - 2.25 | 0.521 |
| Primary school education | 1.88 | -0.03 - 3.16 | 0.055 |
| Poor physical activity | 4.23 | -0.24 - 8.70 | 0.063 |
| Current smoker | -1.88 | -6.00 - 2.23 | 0.370 |
| Body mass index ≥30 kg/m2 | -0.66 | -2.70 - 1.37 | 0.523 |
| Poor diet | 2.78 | -1.41 - 6.98 | 0.194 |
| Fasting glucose ≥126 mg/dL | -0.66 | -2.54 - 1.21 | 0.487 |
| Total cholesterol ≥240 mg/dL | 1.03 | -1.35 - 3.41 | 0.395 |
| /cut1 | -3.47 | -8.75 - 1.79 | … |
| /cut2 | 5.54 | 0.43 - 10.7 | … |
| /cut3 | 11.7 | 5.42 - 18.1 | … |
*Likelihood ratio versus ordinal logistic model: Chi square= 218.94; Prob>chi square= 0.001*. *Statistically significant result
DISCUSSION
This population-based prospective longitudinal study, conducted in community-dwelling older adults of Amerindian ancestry living in rural Ecuador, shows a little contributory role of BP levels on WMH progression after more than six years of follow-up. Study results aligned with some reports coming from people living in urban centers of developed countries, (6)(7) and at the same time, fill a gap on the knowledge of WMH progression among Amerindians living in remote rural settings.
Other studies have shown that WMH severity at baseline - and not high BP levels - is the most important predictor of WMH progression. (6) This was not the case of our study, in whom the rate of WMH progression was similar across groups of individuals with different grades of WMH severity at baseline.
The association between the presence of non-traditional risk factors and WMH progression has also been demonstrated in some studies, although there is no solid information on these relationships. More information is needed for a better understanding of risk factors linked to WMH progression in different populations. (12)(13)
This study has limitations. The SARS-CoV-2 pandemic struck Atahualpa from the first trimester of 2020, resulting in a high incidence rate of premature mortality among older adults. (14) In addition, several individuals left the village or declined consent for the practice of the follow-up MRI. These events suppose a selection bias. Likewise, CVH metrics (including BP) used for analyses were measured at baseline and this may lead to over or underestimation of our findings. Nevertheless, the population has been closely followed and almost all individuals had repeated CVH metrics determinations over the study years. Our records did not identify significant changes in CVH metrics with the exception of a transient decline in physical activity and dietary habits among older adults during the past year as a result of the pandemic. (15) In addition, the treatment gap precluded assessment of the impact of antihypertensive medications on WMH progression. It is also possible that some unmeasured confounders may have been responsible for at least part of the findings of the present study. Despite these limitations, the study has several strengths that include the population-based design, the homogeneity of the study population, the systematic assessment of CVH metrics by means of uniform and standardized protocols, and the practice of baseline and follow-up MRIs using the same equipment and protocols.
Our findings suggest that WMH progression may occur irrespective of BP levels and other traditional risk factors, and should encourage the search for other risk factors that may be in the path of progressive subcortical damage of vascular origin.














