IMAGES IN CLINICAL NEUROLOGY
A 66-year-old woman with history of cirrhosis of unknown etiology was evaluated one month after transient loss of consciousness followed by dystonic posturing, abnormal speech and shuffling gate. She had been complaining of chronic fatigue, anorexia and weight loos for the past six months, and referred two episodes of non-traumatic nose bleeding in the past two weeks. On physical examination, the patient had mild jaundice, more noticeable in the conjunctiva (Figure 1). The liver was not palpable and there was no evidence of ascites. Neurological examination revealed dysarthria, postural and action tremor, limb dystonia, ataxia of gait, and bilateral extensor plantar responses. These manifestations were consistent with pallidal Parkinsonism (1) Abdominal ultrasound showed a small echogenic liver with rough margins and splenomegaly. Liver function tests were abnormal and ammonia levels were increased. Slit lamp examination was negative. Brain MRI showed symmetrical lesions in both globus pallidus (Figure 2). This patient has acquired hepatocerebral degeneration unrelated to Wilson disease, a rare condition that must kept in mind when examining patients with chronic live failure that develop neurological manifestations associated with bilateral and symmetrical pallidal lesions (2). These lesions are thought to be related to pallidal necrosis due to accumulation of neurotoxins, not only manganese or ammonia, but to aromatic amino acids that may act as false dopamine neurotransmitters and cause the neurological manifestations (3).
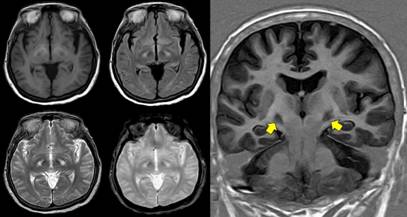
Figure 2 Non-enhanced MRI showing bilateral and symmetrical lesions in the globus pallidus. In the left panel, these lesions are depicted in axial sections of different sequences (T1-weighted, fluid attenuated inversion recovery, T2-weighted, and gradient-echo). The right panel is a coronal section (T1-weighted inversion recovery), where the lesions are clearly visualized (arrows).















