Introduction
Studies in the United States population estimate that 8.7 million women and 2.6 million men suffer from migraines, with moderate to severe disabilities. Of these, 3.4 million women and 1.1 million men experience one or more episodes per month, and women between 30 and 49 years are the most affected group(1) . Latin America, especially Colombia, shows a similar pattern, with an estimated prevalence of 13.8% for women and 4.8% for men, leading many to seek specialized health services or attend emergency centers, impacting the burden and cost of healthcare systems, and the quality of life of the patient(2).
A typical migraine episode consists of a throbbing and unilateral pain accompanied by photophobia, phonophobia and nausea, which may cause disability. Migraines are usually preceded by focal neurological symptoms, called "aura", in up to 30% of patients, typically characterized by any combination of visual, hemisensory or language abnormalities. Each symptom develops over the course of at least 5 minutes and last up to an hour(3)(4)(5).
It is important to establish an adequate clinical approach for migraine sufferers, which should include performing a correct diagnosis and the identification and elimination of exacerbating factors, finally establishing a treatment plan for acute episodes. In addition, it should be determined whether the use of prophylactic therapy is justified(3)(6)(7)(8)(9)(10). Acute episodes are managed according to pain intensity with non-opioid oral analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs)(3)(9) or ergotamine, despite the fact that ergotamine has been overtaken by triptans, considered to be a better choice for the treatment of moderate to severe migraine(3)(11)(12) .
The Colombian Health System offers universal coverage through two affiliation regimens: a contributory regime covered by the worker and the employer and a state-subsidized regime, which includes most medications used in migraine management, such as non-opioid and opioid analgesics, NSAIDs, ergotamine, β-blockers, antidepressants and some triptans (sumatriptan, naratriptan). Given that migraines are a frequently occurring condition that significantly affects the health of those who suffer from them, this study aimed to determine the prescription patterns of antimigraine medications in a Colombian population.
Materials and methods
A cross-sectional study was conducted using a population database of approximately 6.5 million people affiliated with the Colombian Health System contributory regime through six insurers, called Health Promoting Entities [Empresas Promotoras de Salud -EPS]. Prescription data were analyzed based on formulas dispensed from February 1 to April 31, 2018 in all patients with any of the following migraine-related diagnostic codes, according to the International Classification of Diseases, Tenth Revision (ICD-10): G430, G431, G432, G433, G434, and G435.
Data from migraine sufferers of all ages regardless of sex who were seen in medical consultations and whose antimigraine treatment was maintained for at least three months were included. The objective of these criteria was to ensure that patients complied with their treatment in a stable manner, reflecting tolerance and adherence to the medication. For the patients identified with these diagnoses, the data on the dispensation of antimigraine medications, as well as their concomitant treatments, were reviewed. The following variables were collected:
-Sociodemographic: sex, age, and city;
-Pharmacological: antimigraine medications dispensed; their respective doses (and the defined daily dose [DDD]) were used as technical measuring units, considering drugs for the following:
1.Acute management specific to migraines: a) triptans; and b) ergot derivatives;
2.Nonspecific management of migraines: c) NSAIDs; d) acetaminophen; and e) opioids; and
3.Migraine prophylaxis: f) botulinum toxin; g) topiramate; h) β-blockers; and i) valproate. Therapy with j) antidepressants, including tricyclics and selective serotonin reuptake inhibitors, among others, were also considered as prophylaxis(13)(14)(15)(16).
In addition, patients receiving metoclopramide were identified. The medical specialty of the prescriber was identified and whether the medications were administered in monotherapy or combined therapy (defined as having more than one medication for migraine management during the study period, both for acute use and for prophylaxis).
-Concomitant treatment: dispensation of the following risk medications for acute exacerbation(3): a) oral contraceptives; b) hormone replacement therapy; c) nasal decongestants; and d) proton pump inhibitors. In addition, the following medications associated with cardiovascular disease were considered: a) antihypertensives; b) anti-arrhythmics; c) statins; d) vasodilators; e) antiplatelet drugs; and f) antidiabetic drugs.
The statistical package IBM SPSS v 25.0 for Windows was used for data analysis. Descriptive statistics (measures of central tendency, frequencies, and proportions) were used to present the results. Bivariate tests were performed to identify possible relationships between variables, while multivariate binary logistic regression models were applied, considering the administration of prophylactic medications (yes / no) as a dependent variable. The co-variables were those significantly associated with the dependent variable in the bivariate evaluations and those with plausibility to be included. Statistical significance was determined as p < 0.05.
Results
A population of 5973 patients with migraine who were prescribed and received medications to treat this condition was identified. A significant female prevalence was found (n = 4859; 81.3%), and the study population had an average age of 37.7 ± 14.5 years (range: 10.1 - 89.6 years). Bogotá registered the greatest number of treated patients (n = 2408; 40.3%), followed by Barranquilla (n = 675; 11.3%), Manizales (n = 472; 7.9%), Cali (n = 360; 6.0%), Medellín (n = 343; 5.7%), Bucaramanga (n = 341; 5.7%), Pereira (n = 277; 4.6%) and 43 other cities (n = 1097; 18.6%).
The main migraine diagnosis associated with the prescription of medications was migraine without aura (n = 2207; 36.9%), followed by migraine with aura (n = 1697; 28.4%), status migrainosus (n = 906; 15.2%), complicated migraine (n = 805; 13.5%), other migraines (n = 406; 7.7%) and unspecified migraines (n = 212; 3.5%).
A total of 92.8% (n = 5545) of the patients were treated by general physicians during the study period, 436 patients had a neurology consultation (7.3%), 116 were treated by internal medicine practitioners (1.9%), 77 were treated by psychiatry practitioners (1.3%), and 636 (10.6%) were treated by other specialists.
Regarding the management of migraines during acute episodes, 44.1% (n = 2632) of the patients used specific therapies during the observation months, especially ergotamine (n = 2513; 42.1%) and triptans, although at a lower proportion (n = 132; 2.2%). Some patients were prescribed ergotamine or triptans in different months (n = 13). A total of 68.8% (n = 4111) of the patients had nonspecific acute management, mainly with NSAIDs (n = 3112; 52.1%), followed by acetaminophen (n = 1836; 30.7%), and at a lower proportion, opioids (n = 292; 4.9%) (Table 1). A considerable number of cases were prescribed more than one NSAID or a combination of two or more analgesics. In total, 85.4% (n = 5101) of the patients received specific or nonspecific treatment for acute episodes, 51.7% (n = 3087) had exclusively acute management drugs and 12.6% (n = 752) received only prophylactic therapy.
Table 1 Drugs for the management of acute episodes used in 5973 patients diagnosed with migraine, Colombia, 2018.
| Medication | Prescriptions/users | Prescribed doses (mg/day) | DDD† | F:M ratio | Mean age | ||
|---|---|---|---|---|---|---|---|
| # Patients | % | Mean | Median | ||||
| Acute management therapy | |||||||
| Analgesics | |||||||
| Naproxen | 2542 | 42.6 | 803.9 | 750.0 | 1.61 | 4.4 | 35.6 |
| Acetaminophen | 1836 | 30.7 | 1467.1 | 1500.0 | 0.49 | 5.2 | 40.1 |
| Ibuprofen | 569 | 9.5 | 1314.9 | 1200.0 | 1.10 | 4.4 | 35.0 |
| Diclofenac | 368 | 6.2 | 120.8 | 125.0 | 1.21 | 5.5 | 36.9 |
| Tramadol | 282 | 4.7 | 40.2 | 33.3 | 0.13 | 4.4 | 41.4 |
| Acetylsalicylic acid | 14 | 0.2 | 892.9 | 500.0 | 0.30 | 6.0 | 40.9 |
| Morphine | 10 | 0.2 | 22.3 | 10.0 | 44.8 | ||
| Oxycodone | 4 | 0.1 | 22.5 | 20.0 | 0.30 | 3.0 | 40.2 |
| Buprenorphine | 3 | 0.1 | 46.3 | ||||
| Celecoxib | 3 | 0.1 | 200.0 | 200.0 | 1.00 | 51.4 | |
| Meloxicam | 3 | 0.1 | 15.0 | 7.5 | 1.00 | 51.2 | |
| Etoricoxib | 1 | 0.0 | 90.0 | 90.0 | 1.50 | 0.0 | 67.8 |
| Indomethacin | 1 | 0.0 | 100.0 | 100.0 | 1.00 | 33.0 | |
| Methadone | 1 | 0.0 | 40.0 | 40.0 | 1.60 | 74.2 | |
| Oxaprozin | 1 | 0.0 | 600.0 | 600.0 | 0.67 | 70.4 | |
| Specific therapy | |||||||
| Ergotamine / Caffeine* | 2513 | 42.1 | 2.2 | 2.0 | 0.56 | 4.2 | 36.3 |
| Sumatriptan | 58 | 1.0 | 65.7 | 50.0 | 4.8 | 44.1 | |
| Naratriptan | 40 | 0.7 | 2.9 | 2.5 | 1.16 | 12.3 | 42.6 |
| Zolmitriptan | 33 | 0.6 | 7.7 | 6.7 | 3.07 | 32.0 | 43.9 |
| Metoclopramide | 1140 | 19.1 | 14.9 | 10.0 | 0.50 | 4.7 | 34.2 |
*Ratio between the mean daily dose prescribed and the defined daily dose (DDD). NOTE: The DDD used is associated with the main indication of the drug, and not with the specific indication or dose of migraine. F:M ratio = female:male ratio. Doses according to ergotamine
A total of 2766 patients (46.3%) were prescribed migraine prophylaxis medications, of which 33.9% (n = 2024) received monotherapy, 9.2% (n = 551) received two medications, 2.5% (n = 147) received three, 0.6% (n = 35) four, and nine patients received five or more medications during the observation months. Anti-epileptics (n = 1207; 20.2%), tricyclic antidepressants (n = 950; 15.9%), selective serotonin reuptake inhibitors and dual antidepressants (n = 732; 12.3%) and β- blockers (n = 488; 8.2%) were the most frequently prescribed drugs (Table 2).
Table 2 Medications used for prophylaxis in 5973 patients diagnosed with migraine, Colombia, 2018.
| Medication | Prescriptions/users | Prescribed doses (mg/day) | DDD† | F:M ratio | Mean age | ||
|---|---|---|---|---|---|---|---|
| # Patients | % | Mean | Median | ||||
| Prophylaxis therapy | |||||||
| Antiepileptics | |||||||
| Valproic acid | 615 | 10.3 | 373.3 | 250.0 | 0.25 | 4.0 | 36.9 |
| Topiramate | 486 | 8.1 | 56.8 | 50.0 | 0.19 | 7.7 | 46.1 |
| Divalproate | 202 | 3.4 | 457.0 | 500.0 | 0.30 | 5.1 | 41.7 |
| Magnesium valproate | 3 | 0.1 | 466.7 | 400.0 | 0.31 | 42.8 | |
| Antidepressants | |||||||
| Amitriptyline | 609 | 10.2 | 28.3 | 25.0 | 0.38 | 6.2 | 38.7 |
| Imipramine | 367 | 6.1 | 22.6 | 25.0 | 0.23 | 5.7 | 41.3 |
| Fluoxetine | 297 | 5.0 | 24.0 | 20.0 | 1.20 | 6.2 | 43.0 |
| Trazodone | 275 | 4.6 | 60.6 | 50.0 | 0.20 | 5.1 | 45.8 |
| Sertraline | 184 | 3.1 | 65.0 | 50.0 | 1.30 | 6.1 | 48.1 |
| Escitalopram | 41 | 0.7 | 15.3 | 10.0 | 1.53 | 9.3 | 47.3 |
| Duloxetine | 21 | 0.4 | 61.4 | 60.0 | 1.02 | 20.0 | 46.9 |
| Venlafaxine | 13 | 0.2 | 147.1 | 75.0 | 1.47 | 12.0 | 50.1 |
| Mirtazapine | 12 | 0.2 | 30.0 | 26.3 | 1.00 | 5.0 | 54.8 |
| Fluvoxamine | 10 | 0.2 | 166.7 | 200.0 | 1.67 | 1.0 | 46.0 |
| Desvenlafaxine | 8 | 0.1 | 62.5 | 50.0 | 1.25 | 7.0 | 44.5 |
| Paroxetine | 6 | 0.1 | 21.7 | 20.0 | 1.08 | 2.0 | 55.5 |
| β-blockers | |||||||
| Propranolol | 309 | 5.2 | 59.1 | 40.0 | 0.37 | 6.9 | 38.7 |
| Metoprolol | 185 | 3.1 | 76.0 | 50.0 | 0.51 | 3.7 | 50.0 |
| Botulinum toxin* | 129 | 2.2 | 8.9 | 46.0 |
*Ratio between the mean daily dose prescribed and the defined daily dose (DDD). NOTE: The DDD used is associated with the main indication of the drug, and not with the specific indication or dose of migraine. F:M ratio = female:male ratio. Botulinum toxin type A
The mean age of the patients receiving prophylaxis was higher than those without this treatment (41.5 vs. 34.4 years; p < 0.001). In the multivariate model, it was found that being 35 or older, being a woman, receiving concomitant treatment and being treated by a neurology specialist or internal medicine practitioner increased the probability of receiving a prophylactic prescription. In turn, the use of NSAIDs and specific acute therapy for migraine were associated with a lower probability of receiving prophylaxis (Table 3).
Table 3 Variables associated with the use of prophylactic medications for migraine in binary logistic regression models, Colombia, 2018.
| Variables | Sig. | OR | 95% CI | |
|---|---|---|---|---|
| Lower | Upper | |||
| Age ≥ 35 years | <0.001 | 1.86 | 1.66 | 2.08 |
| Female sex | <0.001 | 1.41 | 1.22 | 1.63 |
| Use of: | ||||
| NSAIDs | <0.001 | 0.66 | 0.59 | 0.74 |
| Specific therapy * | <0.001 | 0.51 | 0.45 | 0.57 |
| Any comedication | <0.001 | 1.59 | 1.41 | 1.80 |
| Be attended by: | ||||
| General practitioner only | <0.001 | 0.70 | 0.59 | 0.84 |
| Neurology | <0.001 | 19.02 | 11.03 | 32.78 |
| Internal Medicine | <0.001 | 3.69 | 2.21 | 6.15 |
*Sig: Significance; OR: Odds ratio; 95 % CI: 95 % confidence interval. NSAIDs: Nonsteroidal anti-inflammatory drugs. Specific therapy for migraine: triptans and ergotamine
It was found that 67.2% (n = 4014) of all patients were receiving combination therapy, mainly with two (n = 2056; 34.4%) or three (n = 1158; 34.4%) drugs. Regarding acute specific therapy, 78.0% (n = 2054 out of 2632 cases) of these patients were administered combined management, while those receiving prophylaxis accounted for 82.4% (n = 2280 out of 2766 subjects with prophylaxis). Figure 1 shows the main molecules assessed by the study and their distribution according to combined therapy.
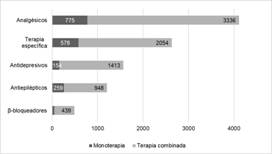
Figure 1 Prescription pattern of the primary drugs for migraine patients, either monotherapy or combined, Colombia, 2018.
In general, the dose of each drug administered for the treatment of migraines was lower than the DDD. However, for drugs such as fluoxetine, escitalopram, ibuprofen and naproxen, the dose was higher than recommended (Tables 1 and 2).
Concomitant medications (co-medications)
It was found that 31.3% (n = 1871) of patients received concomitant medications for treating other comorbid conditions, where proton pump inhibitors (n = 856; 14.3%) and statins (n = 435; 7.3%) were administered with higher frequency. The most often prescribed antihypertensives were angiotensin II receptor blockers (ARBs), which were administered to 403 patients (6.7%), followed by calcium channel blockers (n = 171; 2.9%). A total of 420 women (7.3%) received hormone therapy, including contraceptives (n = 392; 6.6%) and estrogen replacement (n = 38; 0.6%), while only 67 patients (1; 1%) had anti-flu medications / nasal decongestant dispensations.
Discussion
In the present study, outpatient care prescription patterns of different medications for acute management and prophylaxis of migraine were identified in a group of Colombian patients. The results can be used by physicians responsible for the treatment of migraines and by decision-makers to improve the quality of antimigraine prescriptions.
The population had a marked female predominance, which is consistent with several previous studies(3)(17)(18)(19). In addition, the average age close to 40 years old also agrees with the different epidemiological reports worldwide, where it is estimated that the pathology has higher prevalence in patients between 25 and 55 years of age(1)(3)(20)(21)(22) .
Regarding the diagnoses, the proportion of migraine without aura (37%) was similar to a previous study in the Colombian population (43%)(23) . On the other hand, only 28% of the patients had a record of migraine with aura compared to 50% previously reported for Colombia(23); however, it has been described that worldwide, one-third of migraine sufferers present with aura neurological symptoms(20). These differences may be due to the study technique because the diagnoses in the present study were obtained from ICD-10 records, while in the previous Colombian study, an interview with a neurologist was conducted in each case.
The high proportion of patients attending a general practitioner was expected for the Colombian health system. This value is higher than other studies, where visits to general practitioners or internists do not exceed 70%.(24). In contrast, neurology consultations were much lower than reported in the United States by Ford et al., where this specialty treated 30% of patients with episodic migraines and up to 65% with chronic migraines.(24). This may indicate the limited access to this type of specialty for Colombian patients. Other authors have found differences in prescriptions in relation to the caregiver, as was seen for some medications included in this study(25) .
Regarding acute management, greater than 85% of patients were using some medication for this purpose. This finding is consistent with other international studies. In a report of migraine sufferers in the USA, it was found that more than 90% had drug prescriptions for the acute management of their condition(24) . However, the differences are marked in terms of the medication administered, given that the study by Ford et al. found that in acute management, mainly triptans and NSAIDs were used. In our study, ergotamine was found to be highly used(24). The use of ergotamine is not always straightforward, and its high consumption could be interpreted as inadequate, especially considering that a study conducted in Colombia found that physicians had difficulties in prescribing this medication(12).
Data from the current study showed a relatively low use of prophylactic drugs compared to that of the US population, where 52% of patients with episodic migraines and up to 95% with chronic migraines had prophylactic drug prescriptions(24). In the US study, topiramate predominated as a prophylactic drug of choice, which contrasts with our findings where valproate was the most widely administered antiepileptic, although both are recommended by the migraine management guidelines(16).
In the present study, a high proportion of patients were administered antidepressant medications, which can be considered as prophylactic therapy for migraine episodes. However, these medications can also be used for treating depressive episodes and other psychiatric disorders, such as anxiety or panic disorder, which have been frequently described in migraine sufferers(21)(24)(26). Regarding concomitant treatments, a significant number of prescriptions for proton pump inhibitors were found, similar to the findings of other pharmacoepidemiologic studies of neurological drugs in the Colombian population(27).
The low number of prescriptions of drugs for other chronic diseases (such as antihypertensives) is consistent with the age range of migraine sufferers. However, these and other cardiovascular comorbidities should be considered, given that certain acute management prescriptions, and the presence of migraine itself, have been associated with an increased risk of suffering cardiorespiratory and cerebrovascular disorders(20)(28).
There was a low frequency of prescription for contraceptives and hormone replacement therapy. Nevertheless, physicians should be cautious because these medications may present a wide range of adverse effects, ranging from changes in headache episode frequency to cardiovascular events, especially thromboembolism, for which the benefit of their use may be overcome by the risk entailed(29).
The present study has certain limitations. It is based on drug administration records for migraine patients, and clinical characteristics such as onset age of symptomatology, pain location, intensity, aura type, and therapy effectiveness are not available. In addition, the consumption of over-the-counter medications is unknown, which may affect the proportion of use for both acute care and prophylactic drugs(30)(31). We did not conduct a cost analysis of the therapies or other economic implications directly or indirectly related to migraines, such as emergency service care or work absenteeism. Strengths of this study are that it was based on strict records of drugs that were dispensed and included data regarding the delivered quantity and dose and of the treating physician.
Conclusions
The findings of the present study show that migraine patients are predominantly prescribed medications for the acute management of their symptoms, and these were mainly for ergotamine, NSAIDs and acetaminophen, with a very low proportion of triptans. For prophylactic therapy, the prescription of antiepileptics (valproic acid and divalproate) and antidepressants (mainly amitriptyline) predominated, while the use of β-blockers, such as propranolol, was very low. It is important that treating physicians review the need for prophylaxis, avoiding the overuse of acute management therapies that may have limited effectiveness and be associated with important adverse events, particularly for ergotamine. Further studies are needed to verify the effectiveness of treatments and evaluate other outcomes of interest, such as the costs and disabilities associated with these conditions.














