INTRODUCTION
The association between the neck circumference (NC) and obstructive sleep apnea (OSA) has been extensively investigated, with inconsistent results(1)(2)(3)(4)(5)(6)(7)(8)(9)(10)(11)(12)(13). Such inconsistencies are probably related to differences in study designs or to diverse ethnicity of study populations. Some studies found that women have greater fat pads lateral to the pharynx, which are supposed to restrict the upper airway facilitating the occurrence of OSA; however, OSA is more frequent in men(2)(9)(10)(11). This paradox could be related to different phenotypic neck composition or to job-related differences across genders, influencing the amount of fat in the neck and the relationship between NC and OSA.
Neither the association between NC and the apnea-hypopnea index (AHI), nor the effect modification of gender in this association, have been evaluated in Amerindians. In this study, we aimed to assess the effect modification of gender in the association between NC and AHI in stroke-free older adults of Amerindian ancestry.
METHODS
Study population: The study was conducted in Atahualpa, a rural Ecuadorian village, where previous studies on sleep-disordered breathing have been conducted(14)(15). The population is homogeneous regarding race/ethnicity and living conditions. Most men work as artisan carpenters and most women are homemakers. These job-related consistencies make Atahualpa an optimal setting for studying the effect modification of gender in certain associations related to physical activity. In Atahualpa, as well as in other rural villages, there is no retirement, and men continue working despite advancing age. The Amerindian ethnicity of residents is supported by their phenotypic characteristics, including an olive-moderate brown skin (Type IV in the Fitzpatrick scale), dark brown eyes and hair, short stature, and a predominantly elliptic hard palate (16). The IRB of Hospital-Clínica Kennedy, Guayaquil, Ecuador (FWA 00006867) approved the study.
Inclusion criteria: This study included Atahualpa residents aged ≥60 years fulfilling the following criteria: 1) a single-night polysomnography (PSG) for assessment of the apnea-hypopnea index (AHI); 2) a brain MRI for assessment of the total cSVD score; 3) a neurological examination to confirm an overt stroke-free status; and 4) clinical interviews and procedures to assess cardiovascular risk factors, the NC, and the presence of nasal septum deflection.
Main variables investigated: The NC was used as the main independent variable, gender as a second causal (effect modifier) variable, and the AHI as the outcome or dependent variable. The NC (in centimeters) was measured with individuals on the seated position, with a stretch-resistant tape placed immediately above the cricoid cartilage and perpendicular to the long axis of the neck. The AHI calculated the number of apnea/hypopnea events divided by the number of sleep hours, by means of a single-night PSG done at the sleep unit of the Atahualpa Project Community Center. PSGs were performed with the use of an Embletta® X100™ (Embla Systems, Inc; Thornton, CO, USA). A board-certified sleep medicine neurologist, blinded to other information, reviewed raw data and interpreted all exams upon recommendations of the American Academy of Sleep Medicine scoring guidelines (17).
Covariates investigated: Cardiovascular risk factors, nasal septum deflection (deviation of the septum ≥5mm away from the midline), the total cerebral small vessel disease (cSVD) score, and the mean O2 saturation (assessed by PSG) were selected as confounding variables.
Cardiovascular risk factors were assessed according to the American Heart Association (18). Poor physical activity was defined in individuals referring no moderate and vigorous activity, a poor body mass index if ≥30 kg/m2, a poor blood pressure if ≥140/90 mmHg, a poor fasting glucose if ≥126 mg/dL, and poor total cholesterol blood levels if ≥240mg/dL.
Neuroimaging signatures of cSVD were assessed by means of a Philips Intera 1.5T MRI machine (Philips Medical Systems, Eindhoven, the Netherlands), following standards for research on cSVD (19). For calculating the total cSVD, each neuroimaging signature was given 1 point if present, for a maximum score of 4. Points were assigned to white matter hyperintensities if they were moderate-to-severe according to the modified Fazekas scale, to cerebral microbleeds and to silent lacunar infarcts (respectively) if there was at least one lesion located deep in the brain, and to enlarged basal ganglia-perivascular spaces if >10 of these lesions were present in a single slice in one side of the brain (20).
Statistical analyses: Data analyses are carried out by using STATA version 15 (College Station, TX, USA). In univariate analyses, continuous variables were compared by linear models and categorical variables by x 2 or Fisher exact test as appropriate. Using a generalized linear model with gender included as an effect modifier, we evaluated whether gender affected the association between the NC and the AHI (dependent variable), after adjusting for the aforementioned confounders. Using the same model, we obtained AHI marginal means of individuals stratified into percentiles of NC stratified by gender.
RESULTS
A total of 190 individuals fulfilled inclusion criteria. The mean age was 71.1±7.6 years (median age: 70 years, age range: 60 to 95 years) and 122 (64%) were women. A body mass index ≥30 kg/m2 was noticed in 41 (22%) persons, blood pressure ≥140/90 mmHg in 87 (46%), fasting glucose ≥126 mg/dL in 60 (32%), total cholesterol levels ≥240 mg/dL in 28 (15%), poor physical activity in 13 (7%), nasal septum deflection in 30 (16%), and the mean value of O2 saturation was 94.9±4.5%. The total cSVD score was 0 points in 111 individuals (58%), 1 point in 44 (23%), 2 points in 25 (13%), and 3-4 points in 10 (5%). The mean NC was 35.2±3.1 cm (median NC: 35cm), and the mean value of the AHI per hour was 11.9±12.6 (median AHI: 7.1 episodes/hour).
Table 1 depicts the characteristics of participants across men and women. A body mass index ≥30 Kg/m2 was more common in women, and nasal septum deflection in men. The mean NC (37.4±2.6 versus 34±2.5 cm; p<0.001) as well as the mean AHI (14.4±14.5 versus 10.5±11.1 episodes/hour; p=0.039) were greater in men than in women. (Table 1)
Table 1 Characteristics of study participants according to gender (univariate analyses).
| Variable | Total series (n=190) | Men (n=68) | Women (n=122) | p value |
|---|---|---|---|---|
| Age, years, mean ± SD | 71.7 ± 5.7 | 69.8 ± 8.4 | 71.9 ± 8.4 | 0.068 |
| Body mass index ≥30 Kg/m2, n (%) | 41 (22) | 6 (9) | 35 (29) | <0.001* |
| Blood pressure ≥140/90 mmHg, n (%) | 87 (46) | 32 (47) | 55 (45) | 0.793 |
| Fasting glucose ≥126 mg/dL, n (%) | 60 (32) | 24 (35) | 36 (30) | 0.411 |
| Total cholesterol ≥240 mg/dL, n (%) | 28 (15) | 7 (10) | 21 (17) | 0.197 |
| Poor physical activity, n (%) | 13 (7) | 2 (3) | 11 (9) | 0.141 |
| Nasal septum deflection, n (%) | 30 (16) | 21 (31) | 9 (7) | <0.001* |
| Small vessel disease score 0 points, n (%) | 111 (58) | 41 (60) | 70 (57) | 0.696 |
| Small vessel disease score 1-2 points, n (%) | 69 (36) | 24 (35) | 45 (37) | 0.827 |
| Small vessel disease score 3-4 points, n (%) | 10 (5) | 3 (4) | 7 (6) | 0.699 |
| O2 saturation (%), mean ± SD | 94.9 ± 4.5 | 94.7 ± 7.2 | 95.1 ± 1.8 | 0.561 |
| Neck circumference (cm), mean ± SD | 35.2 ± 3.1 | 37.4 ± 2.6 | 34 ± 2.5 | <0.001* |
| Apnea hypopnea index (per hour), mean ± SD | 11.9 ± 12.6 | 14.4 ± 14.5 | 10.5 ± 11.1 | 0.039* |
* Statistically significant result
A fully-adjusted generalized linear model showed a significant association between NC and AHI (β: 2.19; 95% C.I.: 1.05 - 3.33; p<0.001). As NC increased, average AHI also increased. This model also showed a significant effect modification of gender in the aforementioned association (β: -1.74; 95% C.I.: -3.12 to -0.37; p=0.013). Neither the body mass index nor other confounding variable (with the exception of the mean O2 saturation) attained independent significance in this model. The multivariate probability model with individuals stratified into percentiles of NC showed that men started with lower AHI margins at the 10th percentile of NC, and while both significantly increased, men had a much larger rate of change in the average AHI. Therefore, there were no overlapping 95% C.I. in the marginal means of AHI across men within the 10th, 25th and 50th percentiles of NC when compared to those within the 90th percentile. In contrast, 95% C.I. of AHI score overlapped in women assigned to all percentiles of NC (Figure 1).
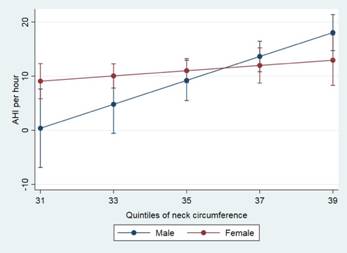
Figure 1 Multivariate probability model with individuals stratified into percentiles of neck circumference (NC) shows that women had significantly higher marginal means of the apnea-hypopnea index (AHI) than men at lower percentiles of NC. In contrast, the association between the NC and the AHI in men with a NC below the 50th percentile is irrelevant.
DISCUSSION
This study shows a significant effect modification of gender in the association between NC and AHI in older adults of Amerindian ancestry, living in a population where most men - as artisan carpenters - have been engaged from their youth in heavy physical work, carrying or lifting heavy wood items. In contrast, women - as homemakers - have not been subjected to that kind of physical activity. These working arrangements may lead us to assume that the percentage of lean tissue (non-fat soft tissue) in the neck of men is different than in women or, in other words, that fat tissue predominates in the neck in women. Such differences could explain the main findings of this study.
The multivariate probability model with individuals stratified into percentiles of NC (Figure 1) shows that women had higher marginal means of AHI than men at lower percentiles of NC, probably because women have more adipose tissue surrounding the pharynx than men irrespective of NC. In contrast, lean tissue may predominate in men (except for those with large necks) and the association between NC and AHI in men with a NC below the 50th percentile is irrelevant.
Studies attempting to assess the association between NC and OSA gave inconsistent results. In one study, fat in the neck did not correlated with OSA severity (5). In others, the association between fat in the neck and OSA was relevant only for men (9)(10)(11). In our study, women at lower percentiles of NC had higher marginal means of AHI than men, which were compensated as NC increased, where marginal means of AHI became slightly greater in men (with overlapping 95% C.I. though), suggesting that the relationship between NC and AHI is more uniform in women (irrespective of NC). The negativity of the β-coefficient of the effect modified variable (gender) in the multivariate probability model strongly suggests that being female captures most of AHI effect.
This study does not evaluate the percentage of parapharyngeal adipose tissue, but job-related differences across men and women might explain the different pattern of the association between NC and AHI across genders, which may not be generalizable to other populations. Another limitation of this study is its cross-sectional design, precluding the assessment of the direction of the relationship between NC and AHI; however, biological plausibility suggests NC as the exposure and AHI as the outcome (the opposite is unlikely). Strengths of this study include the homogeneity of the population, the fact that PSGs were performed in apparently healthy individuals taken from the community, and the models used to assess the effect modification of gender in the aforementioned association. Further longitudinal studies are needed to corroborate our findings.














