Introduction
A potential pathogenetic mechanisms proposed to explain the occurrence of aberrant pneumatization of skull bones is the ball valve mechanism associated with recurrent Valsalva maneuvers. It has also been reported the occurrence of symptom in patients with pneumatoceles with Valsalva maneuvers1. In this view, it is possible that air forced up the Eustachian tube is trapped and gradually spreads into contiguous bones, particularly the temporal squamas and occipital bones.
The obstructive sleep apnea/hypopnea syndrome (OSAHS) has effects on intrathoracic hemodynamics that could be compared with those of a sequence of several repetitive Müller maneuvers alternated with Valsalva maneuvers at the end of each obstructive “apnea complex” (2. Therefore, it is theoretically possible that OSAHS is related to aberrant pneumatization of skull bones, but this association has not been investigated so far. However, it is also possible that in patients with OSAHS, the level of obstruction could be retro-lingual, retro-palatal or both. These levels are below Eustachian tube and thus should not contribute to middle ear pressure. We recently conducted a pilot study in community-dwelling older adults living in Atahualpa (a rural village of Ecuador) to evaluate the practicability of large-scale sleep research in underserved remote populations3,4. As those individuals underwent polysomnography (PSG) and computed tomography (CT) of the head, we aimed to assess the association between OSAHS and aberrant pneumatization of skull bones.
Methods
Methodology of the Atahualpa Project has been detailed elsewhere5. The Institutional Review Board of Hospital-Clínica Kennedy in Guayaquil, Ecuador (FWA 00006867) approved the protocol and the written informed consent form. More than 95% of the population of Atahualpa belongs to the Native/Mestizo ethnic group (Amerindians) and their living characteristics have been detailed elsewhere3,5. Out of 50 randomly selected Atahualpa residents aged ≥60 years that were invited to participate in this pilot study, 40 agreed to undergo single diagnostic night PSG at the sleep unit of the Atahualpa Project Community Center. Individuals were selected by the use of the Random Integer Generator (https://www.random.org/integers/).
PSGs were performed with an Embletta® X100™ Comprehensive Portable PSG System using AASM compliant PSG software. Local nurses received training on PSG data collection, and US certified technicians processed and scored raw data. A board-certified sleep neurologist (P.R.C.) carried out analyses of sleep efficiency, architecture, arousal indexes, apnea/hypopnea index, oxygen saturation, heart rate and motor activity.
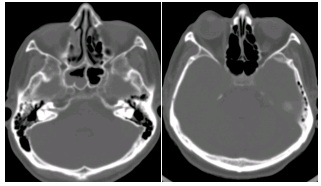
For this study, we focused on the association between the severity of the apnea/hypopnea index with the presence and distribution of pneumatization of intracranial bones, as assessed by CT with bone window settings. Scans were performed with a Philips Brilliance 64 CT scanner (Philips Medical Systems, the Netherlands) at Hospital-Clinica Kennedy, Guayaquil; slice thickness was 3mm with no gap between slices. We defined aberrant pneumatization as the presence of air in non-habitual locations such as the occipital bones and temporal squamas (Figure 1). Two investigators (P.R.C., O.H.D.), blinded to patient-code identification and PSG data, independently read all CTs and determined the presence of aberrant pneumatization. Inter-rater agreement was good (k=0.725, 92% agreement), and discrepancies were resolved by consensus.
Results
Thirty-eight out of 40 participants had adequate PSG recordings and were included in this study. Mean age was 74.5 ± 6.8 years and 25 (66%) were women. The apnea/hypopnea index ranged from 0.2 to 56 (mean 15.7 ± 14.6) episodes per hour. Fifteen persons (39%) had ≥10 episodes per hour and were considered to have OSAHS. There were no differences in the mean age (74.9 ± 7.7 versus 74.2 ± 6.2, p=0.759) or in the percentage of women (60% versus 70%, p=0.728) among persons with and without moderate-to-severe OSAHS. Abnormal pneumatization of skull bones was noticed in six persons, included five out of 15 (33%) with OSAHS and one out of 23 (4%) without (p=0.027, Fisher exact test). Air was found in the temporal squamas in five (bilateral in four), the occipital bones in one, and in both the temporal squamas and the occipital bones in the remaining person.
Discussion
This study shows a significant association between OSAHS and aberrant pneumatization of skull bones. These findings are of potential clinical relevance, since these individuals could be at increased risk of painless fractures from minor trauma or may be prone to develop spontaneous CSF leaks, a complication that has already been reported in association with OSAHS6.
Aberrant pneumatization of skull bones may not be a consequence of OSAHS, but both conditions may share a common pathogenetic mechanism. In this view, the contribution of altered craniofacial anatomy to the upper airway narrowing seen in OSAHS probably explains our findings. In the present study, we have assessed a homogeneous racial population of Ecuadorian natives, in whom we have previously demonstrated an unexpectedly high prevalence of a Friedman’s palate position type IV, which could be genetically determined since Amerindians have a predominantly elliptic hard palate7. Whether such morphological differences account for the high prevalence of aberrant pneumatization of skull bones by changing resistance patterns through the upper airway is unknown.
A limitation of this study is the small sample size, precluding the construction of regression models adjusted for potentially confounding variables. In addition, its cross-sectional design does not allow to assess causality. Also, this study only include older adults, and pneumatization of skull bones have probably been long established (before the appearance of OSA). However, the population-based random sampling design together with the use of validated protocols for PSG interpretation and the quality of the CT machine argue for the strengths of our findings, showing that OSAHS and aberrant pneumatization of skull bones might be related. Further longitudinal studies in our population will help to clarify the cause-and-effect of this relationship, and comparisons with people from other race/ethnicities will determine whether Amerindians with OSAHS are prone to develop aberrant pneumatization of skull bones due to genetically determined morphological differences of the skull.