Introduction
Major Depressive Disorder (MDD) is a highly prevalent and disabling psychiatric disorder that affects more than 350 million people worldwide (1)(2). Importantly, nearly half of people diagnosed with MDD live in the South-East Asia region, Western Pacific region, and South America, and MDD is more frequent among women (3). This medical condition has found to be the main cause of suicide mortality around the world and indeed approximately 50% of suicides are associated with MDD (2)(4). Particularly, in Ecuador, 5.6 % population was diagnosed with MDD and it was postulated that this disorder is responsible for 8.3 % total disability occurring in the country, ranking it in 11th in the list of countries with a higher prevalence of MDD in Latin America (2).
Despite the high prevalence and existence of treatments for MDD, roughly less than half of the people affected by this condition in the world receive medical assistance. Remarkably, although MDD prevalence was found to be similar in high-income and low-income and middle‑income countries, there is a large discrepancy between countries is evident in terms of the resources and treatments available (5)(6). In high-income countries, approximately 50-60% of patients receive proper treatment, whereas in low-income countries this event was not observed since approximately less than 10% of patients receive suitable treatment (1,5,6). More importantly, in low-income countries with these limitations, the individuals assume a large proportion of the economic and social burden induced by MDD, due to the absence or ineffectiveness of specialized services of health (7)(8). Additionally, sociodemographic aspects such as stressful life events, poor education, and quality of life may predict the onset of depressive episodes (1).
Therefore, these data underscore a significant concern about the state of mental health of the population, which is purposed to be a critical component of public health and a socioeconomic challenge (2). Within this context, population-based surveys may provide reliable estimates for health care planning, pointing out population groups that are either vulnerable or at greater risk for several disorders, including MDD (9). Given this background, the present study investigated the prevalence of MDD in the population of Portoviejo, Ecuador. The population was hard-hit by an earthquake in 2016 and still faces a range of consequences generated by this event. We hypothesized that the vulnerability of this population would lead to a high prevalence of MDD. To the best of our knowledge, this is the first household survey study conducted to find out the prevalence of MDD and sociodemographic characteristics in the Portoviejo city, Ecuador.
Material and Methods
Study setting and sample
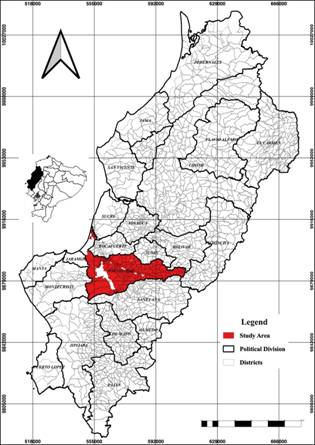
The Province of Manabí is situated in the Occident area of Ecuador, a geographical area known as the Litoral or Costa region. Portoviejo city is the administrative capital of this Province of Manabí and has approximately 329.144 thousand inhabitants and an agroindustry-based economy (Figure 1). Portoviejo has a semi-arid climate and is the third province in the country by extension.
Sample and design
This regional cohort study was performed between August 2018 and October 2019. The study was performed as a household-based survey with a randomized cluster-based sampling process, implemented in three stages in both urban and rural areas of the country: primary sampling units were counties or groups of counties; secondary units were the households, and tertiary units were the adult residents (≥18 years). The probability sampling was used to randomly select eligible adults within sampled households (10), and this strategy ensured the regional representativeness of the study. The total population of Portoviejo in urban and rural zone is approximately 329.144 inhabitants. Of note, the city is divided into 9 urban areas with approximately 264.589 inhabitants (80.39%) and 7 rural areas with approximately 64.555 inhabitants (16.61%). The present study considered an average of each zone to carry out the visits and collect data. Importantly, households that were closed or uninhabited, as well as individuals that refused to answer the interview or those who were not found, were considered losses/refusals, as previously purposed (9).
Data were gathered utilizing a questionnaire that addressed a variety of health-related topics. The present study had an education character, since during the neuroscience discipline of Medicine carrier at Technical University of Manabí, 208 students received a training of a neurologist between March and July of 2018. After theory study of MDD and complete knowledge of questions clinical interviews, the neurologists considered that the students were able to perform the questionnaire. Of note, the data was collected between August 2018 and October 2019. All the interviews were conducted door-a-door to ensure the quality of response. The participants were visited at home and were invited to participate in the study. The students used the informatics program developed by engineers of the Technical University of Manabí, in which interviews were carried out using handheld computers and transferred to a central computer for subsequent data analysis, ensuring data security and confidentiality. The geographical location was indicated by the municipal strategic planning of Portoviejo.
Data description and processing
The initial database comprises a total of 129.633 records from both rural and urban areas. We applied data quality control to remove missing values (NAs) and spurious data. The age of the participants was calculated based on birth dates, and subsequently, a filter was applied:
A id <18(1)
Where A id is the age of the participant in the initial database. After quality control and filtering removal, we were left with a total of 114.239 total cases (88.12%). After filtering, Cronbach’s alpha coefficient (α) test was applied. The internal consistency method based on α allows estimating the reliability of a measurement instrument through a set of items that are expected to measure the same construct or theoretical dimension (11). Results were considered good and acceptable (0.71 - 0.80), good (0.81 - 0.91), and excellent (> 0.90) as previously reported (12).
Measurement of MDD symptoms and co-variables
The positive screening of MDD was evaluated using the Structured Clinical Interview for the Diagnosis of DSM-IV Disorders (SCID), a semi-structured diagnostic tool, which measured the frequency of MDD symptoms (depressed mood, anhedonia, sleep disturbances, tiredness or lack of energy, change of appetite or weight, feeling of guilt or uselessness, problems to concentrating, feeling slow or agitated and having recurrent thoughts about death or suicidal ideation), in the two weeks before the data collection. The presence of five or more symptoms lasting for one week or more, almost every day, except for while suicidal thoughts, was defined as positive for MDD. Importantly, the presence of at least the depressed mood or anhedonia should be present among the symptoms. The MDD severity was described as follows: mild severity (5 symptoms, a minimum for a diagnosis), moderate (6 to 7 symptoms), and severe (8 to 9 symptoms). The co-variables assessed included the geographical area of residence (urban (U)/rural (R)); gender (male (M) and female (F)); age (18-23 (g1); 24-35 (g2); 36-47 (g3); 48-59 (g4); 60-69 (g5); 70-79 (g6); and 80 (g7) years or over) (11); education (none (0); elementary (1); high school (3); bachelor degree (6) and masters or equivalent (7)) (13)(14) marital status (married; separated/divorced; widowed; single); and social security (presence/absence).
Data analysis
The data set consists of many discrete and continuous variables, which facilitates the use of the most frequent analysis techniques, including linear regression analysis and logistic regression analysis. Here, we used descriptive analyses (15)(16) for overall prevalence, socio-demographic and clinical characteristics separated by sex, age, and standard education classification. Furthermore, we used linear regression using the logarithm of the MDD score as a dependent variable and constructed four analytical models
The following linear based model was tested:
InMDD s = a + B 1 * X 1 + B 2 * X 2 + e (2)
Where InMDD s is the logarithm of MDD + 1, a is the constant (intercept), B 1 and B 2 are the linear coefficients, X 1 and X 2 are the variables and, e is the white noise. This model has been used in other studies, although here we used the logarithm of the dependent variable + 1 as used in (19). Finally, odds ratio analyses (18) was performed to provide an estimate (with confidence interval) for the relationship between MDD and ISCED, age groups, and marital status variables. This enables us to examine the effects of variables on that relationship. Also, be a diagnosis performance test indicator.
All statistical analyses were performed using The STATS package version 4.0.2 for Rstudio software. To identify the relationship between education level and marital status with positive cases we use linear regression to fit the log values. Correlation coefficients were determined by correlation analysis at a 5% (p < 0.05) level of significance.
Ethical issues
The study aims were explained to all subjects assuring that their participation was voluntary and anonymous, and their responses would be kept confidential. Personal identifiers had already been removed from the study. Because of the anonymous and retrospective nature of this study, the need for informed consent was waived by the Ethics Committee that approved the study Protocol.
Results
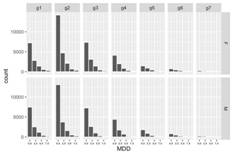
Study area was represented in Figure 1. Age distribution collected from the questionaries’ is summarized in Figure 2. Responders' age ranged from 18 to 90, with the mean being 37.10 (F = 36.68 and M = 37.33). The histogram shows a left-skewed distribution with predominant ages between 20 and 40 years. The sociodemographic parameters indicated a prevalence of secondary schooling (43%) followed by a university degree (34.86%), whereas a total of 6.35% has less than primary or no academic studies. The civil status more prevalent in the present study was single (64%) followed by married (31%), divorced (3%), and widowed (1.8%). Other variables such as social security access (51.09% have access and 48.91% do not access) and Q1 - Q9 questions explanation, frequency, and proportion are evaluated. (Table 1)(Figure 2)
Table 1 Linear and angular coefficients of the multivariate linear models for estimating MDD, considering rural and urban MDD scores variables for Portoviejo.
| Rural | Urban | |||||
|---|---|---|---|---|---|---|
| β | Se | t-value | β | Se | t-value | |
| Intercept | -1.8E-06 | 6.3E-03 | 0.0E+00 | -0.0014 | 0.0178 | -0.0760 |
| q1 | 6.7E-01 | 1.2E+00 | 5.4E-01 | 13.315 | 35.257 | 0.3780 |
| q2 | -9.3E-01 | 2.1E+00 | -4.5E-01 | -24.638 | 59.375 | -0.4150 |
| q3 | -3.1E-01 | 2.7E-01 | -1.2E+00 | -0.3559 | 0.7533 | -0.4720 |
| q4 | 3.9E-01 | 2.0E+00 | 2.0E-01 | 15.326 | 56.323 | 0.2720 |
| q5 | 4.1E-01 | 1.7E+00 | 2.4E-01 | 11.552 | 48.104 | 0.2400 |
| R2 | 0.91 | 0.95 | ||||
| P-value | 0.05142 | 0.02834 |
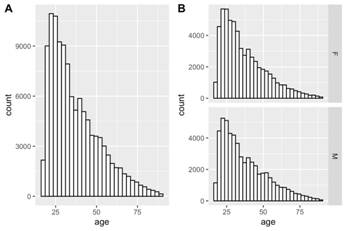
Figure 2 Age distribution of MDD respondents. The histogram shows a left-skewed distribution. A represents total cases and B represents sex facet cases.
The total percentage for MDD found in responders’ population was 8.63%, which was classified as follows: 3.59% for mild MDD, 3.37% for moderate MDD, and 1.67% for severe MDD (supplementary material table 2). Moreover, MDD female cases represented 41.72% of total positive cases when compared with males 58.27% (Figure 3 and supplementary material table 3). Moreover, G2 (24 - 35 years) presented almost 31% of total MMD cases. G7 (> 80) represented ~3% (Figure 2). When it was considerate100% for total MDD cases, mild, moderate, and severe. Single responders had the highest percentage of MDD symptoms (60%) whereas married responders reported 30%. Responders with no access to social security presented uppermost symptoms (55%) when compared to responders with social security (44%) (Table 2)(Figure 3)
Table 2 Odds ratios and 95% *confidence intervals (C.I, lower and upper) of MDD with study level, marital status and age groups.
| ISCED | OR | C.I* (lower) | C.I (upper) | p value |
|---|---|---|---|---|
| 1 | 1.2036*** | 1.0999 | 1.3181 | 5.578E-05 |
| 3 | 0.7290*** | 0.6720 | 0.7917 | 2.072E-13 |
| 6 | 0.7619*** | 0.7014 | 0.8284 | 3.806E-10 |
| 7 | 0.5323 | 0.4568 | 0.6182 | 1.629E-17 |
| Status | ||||
| divorced | 1.0785*** | 0.9489 | 1.2274 | 2.020E-16 |
| married | 0.6317 | 0.5685 | 0.7036 | 6.033E-16 |
| single | 0.6162 | 0.5564 | 0.6840 | 2.759E-18 |
| widowed | 1.9874*** | 1.7217 | 2.2945 | 1.055E-20 |
| Age groups | ||||
| g1 | 1.1839*** | 1.0692 | 1.3099 | 4.783E-03 |
| g2 | 0.7222 | 0.6828 | 0.7640 | 1.789E-29 |
| g3 | 0.7543 | 0.7076 | 0.8039 | 3.810E-18 |
| g4 | 0.8526 | 0.7933 | 0.9160 | 1.304E-05 |
| g5 | 1.1071 | 1.0110 | 1.2108 | 2.869E-02 |
| g6 | 1.3843*** | 1.2389 | 1.5436 | 1.776E-08 |
| g7 | 2.2826*** | 1.9816 | 2.6210 | 4.254E-27 |
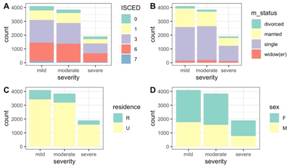
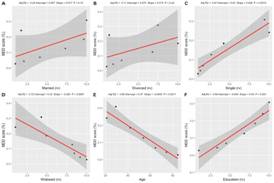
Figure 3 Effect of MDD positive cases for studied variables. Type for International Standard Classification of Education (ISCED) (A), marital status (B), type of residence (C), and sex (B).
Questionaries’ response
After filtering values that satisfied the condition (1) were discarded, a total of 114.240 responders data frame was (88.12%) was then arrange for an evaluation. The alpha coefficient (α) for all variable items was 0.7807213, suggesting that the items have good and acceptable internal consistency (12).
When we evaluated questions separately, we verified that Q6 (whether responders have fatigue or energy loss almost every day) had the highest positive response 24.39%, followed by Q4 (presence of insomnia or hypersomnia almost every day) 23.16%. Concerning the feeling of devaluation or excessive or inappropriate guilt (Q7) (which can be delusional) almost every day (not just self-reproach or guilt for being sick), we found 9.87% of positive response. Regarding the ability to think or concentrate, or indecision almost every day (indicated by the subjective story or by observation of others, Q8), 8 we observed a 14.35% rate of positive results. Ultimately, we measured the recurring thoughts of death (not just fear of dying), recurring suicidal ideation without a specific plan, or a suicide attempt or a specific suicide plan (Q9) (Figure 4). The outcome shows 4.99% of positive responses, which represents 35.98% of the total positive for MDD in the studied population.
There was a suitable agreement between Q1-Q5 and MDD for residence (U-R) scores (Table 1). Both models had a good standard of fit (R2 = 0.91 and 0.95) and a mean p-value of 0.04 for both locations. The statistical analysis indicated a significant positive correlation between marital status and MDD scores (Figure 5), particularly for single (P=0.0014) and widowed (P=0.0097). Moreover, both age and education levels (normalized) were positively correlated with MDD scores (P=0.0011 and P=0.001, respectively). Finally, Table 2 presents odds ratios (ORs) and 95% confidence intervals (CI, upper and lower) for MDD prevalence. Positive and negative groups were here computed. For education level (ISCED), none education, elementary and bachelor’s degree, were more likely to present MDD symptoms with an average OR = 0.89; CI = 0.82 - 0.97. For marital status divorce group OR= 10.78; CI = 0.94 - 1.22 and widowed OR = 1.98; CI= 1.72 - 2.29 were more likely to report MDD. Finally, for age groupers; for those aged 18-23 (OR = 1.18; CI = 1.06 - 1.3) and 60 - 80 (average OR = 1.59; CI = 1.41 - 1.79) prone higher values.
Discussion
Population-based surveys may provide reliable estimates that serve as the basis for health care planning, especially in vulnerable populations as patients with MDD. However, a limited number of population-based surveys focusing on the MDD prevalence had been performed in Ecuador over the past decades. In the present study, we provide the first evidence regarding the prevalence of MDD in a city of Ecuadorian Coast. The results found in our study indicate a high prevalence of MDD, like those published by WHO with a prevalence in Ecuador 5.0% (2)(3)(20). A strength of this study is the large sample size representing a margin of error smaller than 1%, the experimental design door-to-door study, and interviewer training, which are important factors to enable a more precise evaluation.
Exist a lacuna of studies about the prevalence of MDD in Ecuador. Some studies investigating MDD incidence in Ecuadorian populations were performed. Particularly, two studies developed in the indigenous populations from Ecuador showed high rates of moderate and severe MDD symptoms (21)(22). Another study has reported high rated of suicide in adolescents from Ecuador (23) and one work showed mental health problems and related factors in ecuadorian college students (24) Finally, data of WHO has indicated a great prevalence of MDD in Ecuador (2). Despite the importance of MDD, there is evidence about the prevalence of this disorder in the Ecuadorian coast, and thereby our study is pioneering and provides novel evidence about MDD prevalence in Portoviejo as well as the influence of sociodemographic characteristics in this population. According to the data from WHO, 5.6 % of the Ecuadorian population was diagnosed with MDD (2), however, in the present study, we found an MDD prevalence of 8.63% in Portoviejo. It is important to note that this city was hard-hit by the 2016 earthquake and still faces a range of consequences triggered by this event, particularly irreparable damage in the physical infrastructure of the city, which could be related to responders´ vulnerability and prevalence of MDD. This assumption is supported by the higher prevalence of MDD symptoms in responders from the urban area when compared with the rural area, as demonstrated here principal questions (q1 - q5) and average MDD scores close relation. Moreover, a previous report studying the prevalence of MDD symptoms in college students found a smaller index of MDD prevalence (6.2%) when compared with our study (23). Importantly, environmental changes are more likely to be related to the increase of MDD incidence or duration than biological/genetic changes due to the short time frame (1). The Ecuador rates of MDD are similar when compared with low-income and middle-income countries (5,9%) (25)(26).
It is worth to mention that the sensitivity and specificity as the design, methodology, diagnostic tools used, characteristics applied in each study, could affect the results of prevalence of MDD (20)(27). Here, the positive screening of MDD was evaluated using the Structured Clinical Interview for the SCID, one of the most widely used structured diagnostic instruments for assessing mood disorders. The SCID is appropriate for use of adults (age 18 or over) and consists of semi-structured interview validity, in that the order of questions and the initial wording of the questions are prescribed by the instrument, but the interviewer is encouraged to ad-lib, follow-up questions to gather sufficient information to be able to make a clinical judgment as to whether a DSM diagnostic criterion is met (28). In the present study, the severity of MDD was found to be 43-56 % to mild and most respondents had symptoms considered moderate or severe 40-59%. Severe symptoms of MDD are related to suicide risk (29)(30), and the risk of suicide is almost 20 times higher in patients with MDD than in the general population (4). Unfortunately, this behavior increased over time (31), the risk of suicide in Ecuador increased from 165 deaths in 1997 to 286 deaths in 2016, rates increased from 12.7 to 23.3 per 100,000 in the young population (23). It was estimated that around 50% of two 800,000 suicides that occur annually in the world are associated with depressive episodes (2)(28). A meta-analysis revealed that patients with depression have an increased risk of suicide mortality when compared to individuals without depression, reinforcing the notion that this mood disorder is a public health problem (4).
Multiple factors may influence the MDD prevalence, such as family/genetic and environmental factors (30)(32)(33), although neither factor alone cannot be considered risk factors for MDD prevalence. For instance, researches that evaluated age show discrepancies, since the prevalence of MDD was descript lower for younger and older adults (34). However, other studies also reported an increase in MDD symptoms for adolescents and older adults (35)(36). The goal of the current study was to investigate trends in the prevalence of MDD in Portoviejo, particularly in people age 18 years and older. Specifically, we found the prevalence in MDD among the youngest (g1) adults (g2; g3; g3) and oldest (g5; g6; g7) age groups, and the increase was significantly more rapid among the young adult age group (g2, between 24-35 years old) compared with every other age group. Nonetheless, young adults may be impacted by economic-related stress through their family members or in terms of their employment prospects (37).
Previous studies report that MDD is more prevalent in women than men (2)(3)(38). This evidence is consistent with most studies conducted about MDD in low, middle, and high-income countries (20) in remote areas of Ecuador (21)(22). A compelling report studying the global prevalence of MDD in a period of 12-month showed a higher prevalence in females 5.8% compared to males 3.5% (3)(20). However, as opposed to many published studies, here we demonstrated that MDD was more prevalent in men than in women. Considering that in the present study we did not address either daily or sporadic use of tobacco, the abusive use of alcohol as well as health disorders (arterial hypertension, diabetes, and heart disorders), we cannot rule out the interference of these variables in the outcomes. A previous study demonstrated that MDD prevalence in Brazil was associated with smoke, alcohol use, and metabolic disorders (9).
Moreover, it is important to note that these can influence comorbidities further aggravating the problem in individuals with a primary diagnosis of MDD. MDD is associated with a reduction in neurogenesis and cognitive impairment in aged people (39)(40)(41). Moreover, MDD with melancholic characteristics represents less than 1% of depression cases and is more prevalent in men than in women (38)(42). In this sense, Kong et al., (2013) found specific patterns in different sexes, evaluated abnormalities in corticolimbic-striatal morphology in individuals with untreated depression (43). Specifically, pre-limbic abnormalities were found mainly in women, while pre-frontostriatal abnormalities were found mainly in men, pointing to sexual differences in these neuronal circuits (43). These findings may be relevant to sex differences in the presentation of clinical symptoms of depression, such as pre-frontolimbic dysfunction may be related to a higher prevalence of anxiety in women (44), while prefrontal-dysfunction striatal may be related to the higher prevalence of drug abuse among men (45).
The gender gap in MDD has conflicting results while some studies report, that low gender-equity countries have an increased prevalence of depression (46). Other studies showed that the relationship between gender did not differ significantly between high-income and low- to middle-income countries, suggesting that economic development does not explain the varying magnitudes of gender differences in different countries (26). In Ecuador, previous studies demonstrated a higher prevalence of MDD in women (21)(22), while here, our results indicated that men had higher rates of MDD.
Likewise, socio-demographic aspects such as education and quality of life, as well as the different cultural aspects, contribute to such variation. In our study, the prevalence of MDD was associated with a single man that has reached secondary schooling. Marital status seems a factor that influences MDD prevalence, our positive result for single persons represents 60% of interviewed. This result was paralleled by a significant positive correlation between marital status and MDD scores, particularly for single status. Moreover, we also observed a significant positive correlation between widowed status and MDD scores, reinforcing the notion that marital status could contribute to MDD development. Of note, other studies observed depression declined with age for those widowed, separated, and divorced compared to married people (47). It is important to mention, individuals living alone has been descript to risk factor to MDD (48)(49). Furthermore, the protective role of education and sense of mastery in preventing the onset of MDD (50). Here, we found herein that the prevalence of MDD was increased in secondary schooling (represented 43%) when compared with persons that had primary or university degree. We also observed that MDD status was positively correlated with education levels. Noteworthy, several studies showed that the lower degree of education was associated with high rates of MDD (31)(51). Additionally, we demonstrated that age was positively correlated with MDD scores. In fact, studies provided evidence that MDD development seems to be influenced by age, in which it is more prevalent in older adults (52).
Studies focusing on the prevalence of MDD and its association with sociodemographic and clinical characteristics, including other psychiatric disorders, suicidality, impairment, and treatment use, is needed nowadays since this disorder is the number one cause of disability worldwide (10). Additionally, MDD is a social problem that affects individuals of all ages and social spheres, a considerable number of people with a potential need to use health services, which in turn becomes a current socioeconomic challenge (9)(53). In our study, most positive cases of MDD have social security. Although our study did not evaluate socioeconomic status, research shows of lower socioeconomic status are associated with a higher prevalence of MDD (34)(54)(55) and greater odds of chronic MDD (32). On the other hand, our results found a more prevalence of MDD in an urban zone, when compared with rural zone, and distinct populations that present specific characteristics and consequently different prevalence of mental health problems, in Portoviejo case urban zone was severity affected by the 2016 earthquake.
Conclusion
Collectively, our results revealed a high prevalence of MDD in the Portoviejo population, an effect more prominent in man. Of note, the variables living alone, young and resident of the urban zone were found to be the main possible risk factors for developing MDD. However, each culture or country has unique characteristics specific to itself, besides individual factors, socio-cultural features like socioeconomic problems, high unemployment, natural disasters, the prevalence of some chronic diseases, and dependence on another country may lead to an increase in the prevalence of depression.
Strengths and limitations
This study has some limitations: The increase in MDD prevalence may be due to an increase in the incidence of MDD. However, we were not able to examine MDD incidence in the current study due to the variables available for analysis. Additional important information would be gained from examining the incidence of MDD. This study included cross-sectional data that are subject to age >18, in a cohort study. On a related note, cross-sectional data do not allow the examination of cause and effect but indicate paths for future experimental studies. Despite the potential for a questionnaire to assist in the detection of depression, there is needed evidence clinical a screening specific made by a neuroscience professional for accurate diagnosis of MDD. Given the alarming indices found, appears the necessity of new prevalence studies in the city of Portoviejo should be carried out to verify the possible result intervention of public policies that will be adopted and consider the incidence. Furthermore, search regards exposure to other known risk factors associated with MDD, including diabetes mellitus (55), diseases chronic, excessive alcohol consumption and lack of social support (9)(10)(26)(32)(53).